What is aortic disease?
Aortic disease refers to a group of conditions affecting the aorta, which is the largest artery in the body. The aorta carries oxygen-rich blood from the heart to the rest of the body. Aortic diseases can disrupt this crucial function and often involve the weakening, enlargement, or damage to the aortic wall, which can lead to serious complications if untreated.
The aorta is the largest tube (artery) that carries blood cells containing oxygen around the body to your vital organs. The blood cells are pumped from the main pumping chamber called the left ventricle in to the aorta.
The aorta can also be affected by disease and can either generally enlarge (dilate) or balloon with localised enlargement (aneurysm) or can also tear or split (dissection) and these effects can have fatal consequences.
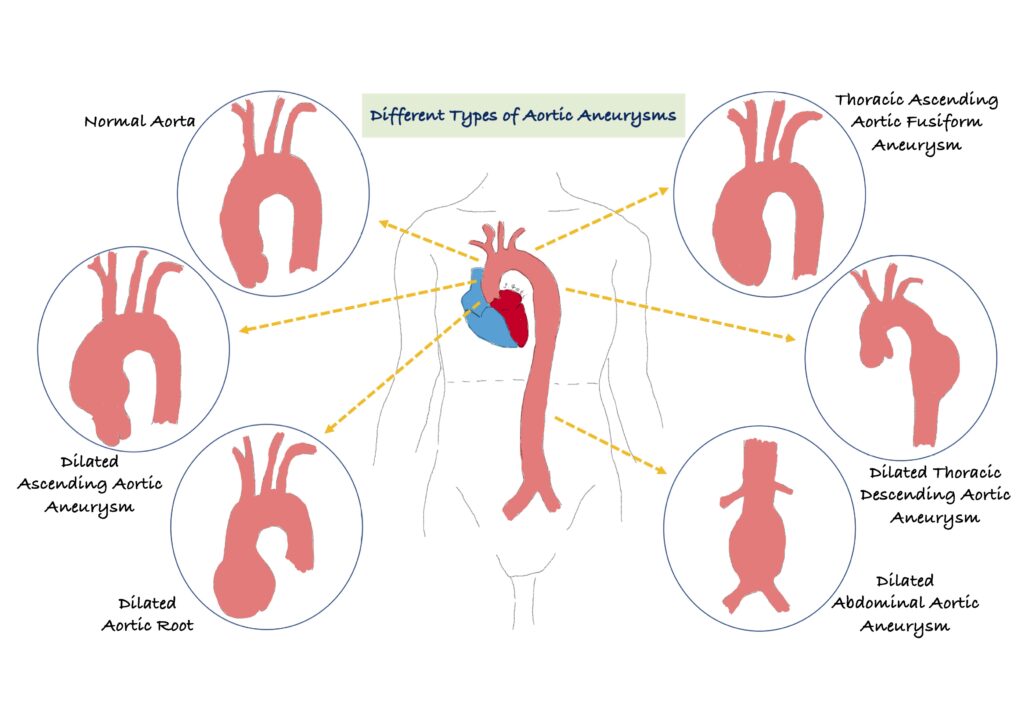
Is there only one type of aortic aneurysm?
The short answer is no, there are three main types of aortic aneurysms. An aneurysm is a weak spot in the wall and cause the aortic tube to bulge like a balloon. The main concern with an aneurysm is that it can rupture and cause severe bleeding which can prove fatal if it is not quickly treated. Aortic aneurysms are classified as
- Abdominal (tummy) aortic aneurysms – as the aorta travels through the tummy it can balloon/bulge. These are also sometimes known as triple A (AAA). Older individuals and those who are long-term smokers are at high risk. The type of symptoms these may present with include an extremely sharp and severe pain which may indicate rupture and this requires emergency treatment and must not be ignored. The other symptom includes pain in the back or in the bellybutton region.
- Thoracic (chest) aneurysms – these occur in the chest; most individuals will not have symptoms but these are usually picked up on imaging such as a Chest X-ray, echocardiogram (ultrasound scan of the heart), CT scan of the chest and/or on an MRI of the heart. If your thoracic aortic aneurysm becomes very large, it can cause discomfort in the chest and even pain between your shoulder blades. If a thoracic aortic aneurysm was found, this would require monitoring on either a 6-monthly or annual basis depending on the size of the aorta. There are many advanced treatments available now when the aorta enlarges significantly, and this includes minimal surgical techniques such as stenting but occasionally you may require complex open-heart surgery to replace the aorta, but this all depends on how complex your disease is. If you want to learn more, please see below.
- Thoracic abdominal (chest and tummy) aneurysms
What causes damage to the aorta?
There are several medical conditions that may damage the aorta and weaken the aortic wall and these can be acquired (environmental) or genetic (running in the family). If these conditions are not treated and monitored, they can put individuals at risk of sudden death, and these include:
- Genetic conditions in young people such as Marfan syndrome
- Connective tissue conditions such as Ehler-Danlos syndrome, Turners syndrome, scleroderma, polychrondritis and polycystic kidney disease
- Trauma or injury to the chest or abdomen
- Hypertension (high blood pressure)
- Atherosclerosis (hardening of the arteries from fatty build up)
What are the treatment options?
Your doctor will initially watch slow growing aortic aneurysms and will advise on lifestyle changes and medications. If the aortic aneurysm is fast-growing it may require surgery and we would advise you are monitored in a specialist clinic.
What is Thoracic aortic aneurysm?
The aorta is the largest tube or vessel in the body and carries the oxygen containing blood round the body. A weakening in the aorta wall can result in an aortic aneurysm (ballooning or bulging) and over time there is a risk it can tear (dissection) or burst (rupture). This would cause life threatening bleeding and place the individual at potential risk of death. Thoracic refers to part of the aorta that runs through your chest.
Once an aortic aneurysm develops it can gradually increase in size and progressively weaken. This would need to be closely monitored in a specialist unit either on a 6-monthly or yearly basis. Treatment for a thoracic aneurysm includes surgery by either repairing it or removing the disease segment and replacing it or a metal mesh coil (stent) can also be inserted if suitable to the diseased aorta and preventing from rupturing.
What causes a thoracic aortic aneurysm?
There are several medical conditions that can cause your thoracic aorta to enlarge or develop an aneurysm and these include:
- Genetic disorders – Marfan syndrome
- Family history
- Diseases of the connective tissue
- Atherosclerosis (hardening of the arteries with fatty plaques)
- Degenerative diseases such as hypertension
- Inflammation of the arteries – your own body develops a heightened immune response to the arteries such as vasculitis
- Infection but this is rare in the Western world.
What sort of symptoms would I experience with a thoracic aortic aneurysm?
These can be really variable; some individuals may not get any symptoms. However, when symptoms do occur, they must be taken seriously and may relate to the location, size and the speed with which the aortic aneurysm is growing or enlarging. Sudden severe pain in the chest radiating into the back could be serious and should not ignored as it could be a life-threatening emergency.
Symptoms to monitor include:
- Pain in the chest or back
- Pain in the neck, jaw, upper back
- Wheezing, coughing and breathlessness due to the aorta pressing on the windpipe
- Hoarseness of the voice
- Difficulty swallowing due to pressure on the gullet pipe.
What tests would I need to diagnose an aortic aneurysm?
A comprehensive evaluation includes a detailed clinical and family history and physical examination. The following tests may be considered:
- Chest X-ray – to check if the cardiac contours on the X-ray image are wide.
- Computed tomography (CT) – this uses X-rays and can take detailed images of the aorta as well as other body structures. Repeats CTs can be associated with accumulated radiation and would not be advised on a 6-monthly basis.
- Magnetic resonance imaging (MRI) – this uses large magnets and radio-frequencies to acquire images of the heart and aorta. This test does not involve radiation and can be used on a 6-monthly basis if needed. This test may not be available in all hospitals.
- Echocardiogram (ultrasound scan) – this uses sound waves to image the heart structure and function. This is good to scan the first part of the aorta as it leaves the heart.
- Aortogram (angiogram) – this is invasive and uses X-rays to assess for aneurysms and narrowing of the blood vessels.
How will my thoracic aortic aneurysm or enlarged aorta be managed?
Once you have been evaluated in a specialist centre, which may include an inherited cardiac condition clinic or an aorta clinic, the initial steps will be baseline tests followed by monitoring with either an MRI or CT. This will allow your doctor to monitor the size and how quickly the aorta is growing. Your clinical surveillance maybe every 6-months or 12-monthly depending on how complex your condition is. Your doctor will also talk to you about making lifestyle changes including giving up smoking, controlling your blood pressure and blood sugars if you are diabetic. They will also give advice on the exercises you should perform to lose weight if you are overweight but also prevent further aggravation of the aortic size. For some individuals, depending on the cause of the aorta enlargement, your doctor may want you to take some medications called beta-blockers, blood pressure pills and to lower your cholesterol levels. Your doctor may also want to start you on a medication called angiotensin receptor blocker such as losartan or irbesartan.
If you get to the stage where you require surgery, these are the options:
- Endovascular aneurysm repair (EVAR) – this is minimally invasive and requires a small cut in the groin and through X-ray machines and specially designed instruments, the surgical team would implant a metal coil meshed stent inside the aorta. Unfortunately, not all thoracic aneurysms can be repaired with this technique and it depends on the type, size and location of your aortic aneurysm.
- Open heart surgery/repair of thoracic aortic aneurysm – if your aneurysm is in the ascending aorta or the arch, you may require an incision/cut through the breastbone. If your aneurysm is also involving damage to the aortic valve, this may also need to be replaced or repaired during your surgery, but your surgeons will discuss your options in more detail. If your aneurysm is in the descending aspects, the incision may extend from the back around the shoulder blade around the side of your rib cage to underneath the breast tissue.
What size of my aorta requires surgery?
The larger your aortic aneurysm the greater the risk of rupture. It is estimated that once your abdominal aortic aneurysm is >5.5cm, this is likely to rupture within 12 months in 3-6 out of 100 people and therefore, surgery would be indicated.
For thoracic aortic aneurysms, the current European Society of Cardiology (ESC) guidelines suggest surgery when the aneurysm is 5cm or more for individuals with a genetic condition placing them at risk of rupture or dissection such as Marfan syndrome and other connective tissue diseases. In non-Marfan patients and in general, the cut-offs are 5.5cm. However, your doctor may start to plan your work-up for surgery earlier than these cut-offs to ensure there is a medical and surgical plan in place for your future care.
What is familial thoracic aortic aneurysm?
Sometimes, a thoracic aortic aneurysm can run in the family and therefore, has a genetic predisposition. We identify this in around 20% of the general population and many people don’t know they have it plus they may not have any symptoms. When there is a genetic element to your condition, your first-degree relatives which includes, parents, siblings and children should be screened for the condition.
There are many genes involved in aortic aneurysm and here are just a few important ones but there is a very long list which can be found on www.omim.org:
1)Fibrillin -1 – this is associated with Marfan syndrome
2) Elastin (ELN) – this is associated with a narrowing above the aortic valve and ascending aortic aneurysms
3) Collagen 1 alpha-1 or 2 (COL1A1/2) – this can cause osteogenesis imperfecta; Ehlers-Danlos syndrome
4) Collagen 3 alpha-1 (COL3A1) – this causes Ehlers-Danlos type 4 which is frequently associated with artery dissection.
5) TGFBR1 and 2 – causes Loeys-Dietz syndrome which is highly penetrating and leads to aortic root and large and medium artery aneurysms
6) SMAD3 (SMAD family member 3) – causes Loeys-Dietz syndrome with osteoarthritis
7) ACTA2 (alpha-smooth muscle actin) – causes familial aortic aneurysms
8) NOTCH1 (notch1) – associated with bicuspid aortic valve with ascending aortic aneurysm
9) JAG1 (jagged1) – associated with aneurysms of brain arteries, narrowing of the aorta and aortic aneurysms
10) PKD1 or 2 (plycystin-1 or 2) – associated with polycystic kidney disease with aneurysms of brain arteries
What is aortic dissection (tear of the aorta)?
The aortic wall is made of 3 layers of tissue, (like sandwich) and a dissection starts with a tear in the inner layer of the wall of the thoracic aorta. Blood then seeps through the layers separating them and progressively weakening the wall and potentially rupturing/bursting (a bit like a soggy sandwich falling apart). Unfortunately, aortic dissection can be life-threatening, and the most common symptom is constant chest pain radiating through to the back between the shoulder blades. The pain can also move from one position to the next. Depending on the location of the dissection, immediate surgery may be required.
Are there any specific triggers or causes of aortic dissection?
The reason why people develop a tear in their aorta is unclear but there are some risk factors we can certainly manage and try to avoid an aortic dissection, and these include:
- Ensuring high blood pressure is treated. If your blood pressure is >140/80mmHg please speak to your GP.
- Genetic conditions such as Marfan syndrome, Ehlers-Danlos syndrome and Turners syndrome. You may need genetic testing for these conditions.
- Inflammation of the aorta called aortitis
- Degenerative disease of the aorta called cystic medial disease
- Atherosclerosis (hardening of the arteries)
- Bicuspid aortic valve with 2 flaps to the valve rather than 3 can also cause enlargement of the aorta
- Trauma/injury
- Narrowing of the aorta called coarctation of the aorta
- Polycystic kidney disease which results in fluid filled pockets in the kidneys. This is a genetic disorder.
Can I exercise with aortic disease?
This is a very good question and it depends on the type of aortic disease you have and how dilated the aorta is. However, in general those who are low risk such as individuals with a bicuspid aortic valve with an aortic dimension of <40mm or Turner syndrome without aortic dilatation can participate in all sports but the preference is endurance rather than power sports.
Individuals who are regarded as intermediate risk such as with Marfan syndrome but without aortic dilatation; people with a bicuspid aortic valve with aorta of 40-45mm or after successful surgery for a bicuspid aortic valve should be advised to avoid high and very high intensity exercise, contact and power sports. Again, the preference for sports should be endurance e.g. running, cycling rather than power sports such as weightlifting.
People who have a moderate aortic dilatation, 40-45mm in Marfan syndrome; 45-50mm in bicuspid aortic valve patients; after surgery for thoracic aorta in Marfan syndromes, the advice is only skilled sports or low-intensity endurance exercise.
Participation in sports as a temporary measure is advised in any individual with a severe aortic dilatation, that is >45mm in Mafan syndrome, >50mm in bicuspid aortic valve or if you have complications after thoracic aortic surgery.
If a young person tragically dies suddenly from a dissected aorta, should first degree blood relatives (siblings, children and parents) be screened to see if this was an inherited condition they may also have?
This is not a straightforward answer as there are a number of causes of an aortic dissection. However, if there was not an obvious cause due to factors such as lifestyle, or a physical event/impact which caused the dissection, then it would be considered good practice for 1st degree blood relates to be screened at an Inherited cardiovascular Conditions Centre to determine if this could have been caused by a genetic condition.